Cervical kyphosis is a spinal condition marked by an abnormal forward curve in the neck. Learn about its causes, symptoms, and treatment options. Find relief and regain mobility.
Cervical kyphosis is a spinal condition characterized by an abnormal forward curvature of the cervical spine, which is the uppermost part of the spine located in the neck region. In a healthy spine, the cervical region typically maintains a gentle inward curve known as lordosis. However, in cervical kyphosis, this normal curvature is disrupted, causing the neck to bend forward more than it should.
Cervical Kyphosis – Basic Understanding
Cervical kyphosis is a spinal condition characterized by an abnormal forward curvature of the cervical spine, which is the uppermost portion of the spine located in the neck region. This condition can have a profound impact on an individual’s posture, neck mobility, and overall quality of life.
- Cervical kyphosis can develop due to various underlying causes, including congenital factors, degenerative changes, poor posture, traumatic injuries, or neuromuscular conditions.
- The symptoms of cervical kyphosis can range from neck pain and stiffness to neurological issues such as numbness, tingling, or weakness in the arms and hands.
- Changes in posture, including a noticeable “hunchback” appearance of the upper back and neck, are often a hallmark of this condition.
- As the cervical spine plays a crucial role in supporting the head and facilitating neck movement, any deviation from its normal alignment can lead to discomfort and functional limitations.
- Diagnosing cervical kyphosis typically involves a combination of clinical evaluation, imaging studies, and specialized tests to assess spinal alignment, nerve function, and associated complications.
- Treatment approaches vary based on the severity of the condition and its underlying causes.
- Conservative management, including physical therapy and bracing, may be effective for mild cases, while surgery is considered for severe cases or when neurological deficits are present.
Summary:
Timely diagnosis and appropriate management are essential to prevent further progression, alleviate symptoms, and enhance the overall well-being of individuals living with cervical kyphosis. This condition underscores the importance of spinal health and the critical role it plays in maintaining a pain-free and functional neck and upper back.
Can Cervical Kyphosis Lead to Complications?
Cervical kyphosis can lead to various complications, especially if left untreated or if it progresses over time. These complications can affect an individual’s overall health and quality of life. Some of the potential complications associated with cervical kyphosis include:
I. Chronic Pain:
- Persistent neck pain and discomfort are common complications of cervical kyphosis. The abnormal curvature of the cervical spine can cause strain on the neck muscles, leading to chronic pain.
II. Nerve Compression:
- Cervical kyphosis can compress the spinal cord or nerve roots in the neck region. This compression can result in symptoms such as numbness, tingling, and weakness in the arms and hands. In severe cases, it can lead to more significant neurological deficits.
III. Muscle Weakness and Atrophy:
- Weakened neck and upper back muscles can develop over time due to the altered spinal alignment. This muscle weakness can impact posture and mobility and may lead to muscle atrophy (wasting) in some cases.
IV. Changes in Posture:
- Cervical kyphosis often causes changes in posture, including a noticeable “hunchback” appearance of the upper back and neck. These changes can affect self-esteem and body image.
V. Difficulty with Balance and Coordination:
- Advanced cervical kyphosis can disrupt the body’s center of gravity, leading to balance and coordination issues. This can increase the risk of falls and related injuries.
VI. Reduced Quality of Life:
- The combination of pain, neurological symptoms, changes in appearance, and functional limitations can significantly reduce an individual’s quality of life. Daily activities and mobility may be compromised.
VII. Respiratory Problems:
- In severe cases of cervical kyphosis, the altered spinal alignment can affect the position of the head and neck, potentially impacting breathing and lung function.
VIII. Difficulty Swallowing:
- Cervical kyphosis can sometimes lead to difficulty swallowing (dysphagia) due to changes in neck anatomy and muscle function.
Summary:
It’s important to emphasize that timely diagnosis and appropriate treatment can help prevent or mitigate these complications. Treatment options, which may include physical therapy, bracing, or surgery, are tailored to the specific needs of the individual and the severity of the condition. Consulting with a healthcare provider or spine specialist is crucial for early intervention and the best possible outcome in managing cervical kyphosis.
Cervical Kyphosis Causes
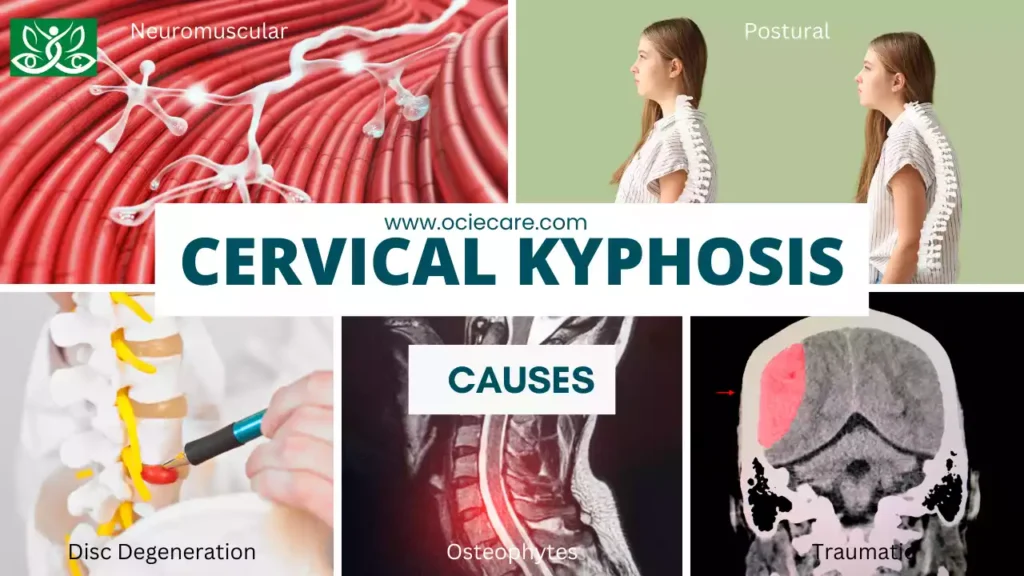
A. Congenital:
- Some individuals are born with structural abnormalities in their cervical spine that predispose them to develop cervical kyphosis.
- These congenital anomalies can include defects in the formation of the vertebrae or abnormal curvature of the spine from birth.
- These pre-existing conditions can lead to an increased risk of developing cervical kyphosis as the individual grows.
B. Degenerative:
Age-related changes in the cervical spine are a common cause of cervical kyphosis, especially in older adults. These changes can include:
I. Disc Degeneration:
- Over time, the intervertebral discs that provide cushioning between the cervical vertebrae can degenerate, leading to a loss of disc height and stability.
- This can contribute to changes in the cervical spine’s alignment.
II. Bone Spurs (Osteophytes):
- The development of bony growths, known as osteophytes or bone spurs, can occur in response to disc degeneration.
- These spurs can impinge on the spinal cord or nerves, potentially causing cervical kyphosis.
III. Postural:
- Prolonged poor posture, especially when using electronic devices for extended periods, has become a common contributing factor to cervical kyphosis.
- This phenomenon is sometimes referred to as “text neck.”
- When individuals consistently crane their necks forward to look at screens, it places excessive strain on the cervical spine, leading to an increased risk of developing kyphotic deformities over time.
IV. Traumatic:
- Traumatic injuries to the neck can result in cervical kyphosis.
- These injuries can include severe neck fractures, dislocations, or traumatic events that damage the cervical spine’s structural integrity.
- Trauma can lead to misalignment or instability of the cervical vertebrae, which may result in an abnormal curvature.
V. Neuromuscular:
- Certain neuromuscular conditions, such as muscular dystrophy or amyotrophic lateral sclerosis (ALS), can affect the muscles that support the spine.
- Weakened or degenerated muscles may be unable to maintain the normal curvature of the cervical spine, leading to kyphotic deformities.
- These conditions can result in muscle atrophy and loss of spinal stability.
Summary:
It’s important to note that cervical kyphosis can develop from a combination of these factors or be influenced by multiple causes simultaneously. Additionally, early diagnosis and appropriate treatment are essential to manage cervical kyphosis effectively, regardless of its underlying cause. Treatment plans are often tailored to address the specific factors contributing to the condition in each individual case.
Cervical Kyphosis Symptoms

I. Neck Pain and Stiffness:
- Individuals with cervical kyphosis often experience neck pain, which can vary in intensity.
- This pain is typically localized to the neck region and may be described as a dull ache or discomfort.
- Stiffness in the neck can make it challenging to move the head freely.
II. Reduced Neck Mobility:
- Cervical kyphosis can limit the range of motion in the neck, making it difficult to perform simple tasks like turning the head to look around, tilting the head, or rotating the neck.
- This restriction in neck mobility is often due to the abnormal curvature of the cervical spine.
III. Headaches:
- Some individuals with cervical kyphosis may experience headaches, which can result from tension in the neck and surrounding muscles.
- These headaches may be localized to the back of the head or radiate to other areas.
IV. Numbness, Tingling, or Weakness in the Arms and Hands (due to nerve compression):
- Nerve compression in the cervical spine, often caused by the abnormal curvature, can lead to neurological symptoms in the upper extremities.
- These symptoms may include numbness (loss of sensation), tingling sensations (paresthesia), or weakness in the arms and hands.
- The severity of these symptoms depends on the extent of nerve compression.
V. Muscle Weakness or Atrophy:
- Over time, cervical kyphosis can lead to muscle weakness in the neck, shoulders, and upper back.
- Weakened muscles may struggle to support the spine’s abnormal curvature.
- In severe cases, muscle atrophy (wasting) can occur, resulting in a loss of muscle mass and strength.
VI. Changes in Posture, Including a “Hunchback” Appearance:
- One of the hallmark signs of cervical kyphosis is a noticeable change in posture.
- The abnormal forward curvature of the cervical spine can cause a “hunchback” appearance, where the neck and upper back bend forward more than normal.
- This change in posture can be visible and may impact an individual’s self-esteem and self-image.
VII. Difficulty with Balance and Coordination:
- In advanced cases of cervical kyphosis, individuals may experience difficulty with balance and coordination.
- The altered spinal alignment can affect the body’s center of gravity, making it challenging to maintain balance while standing or walking.
- This can increase the risk of falls.
Summary:
It’s important to recognize that the severity and combination of symptoms can vary among individuals with cervical kyphosis. Additionally, timely diagnosis and appropriate treatment are essential to alleviate these symptoms, prevent further progression, and improve the patient’s overall quality of life. Management plans are tailored to address the specific needs and circumstances of each patient.
Clinical Characteristics and Diagnostic Approaches of Cervical Kyphosis
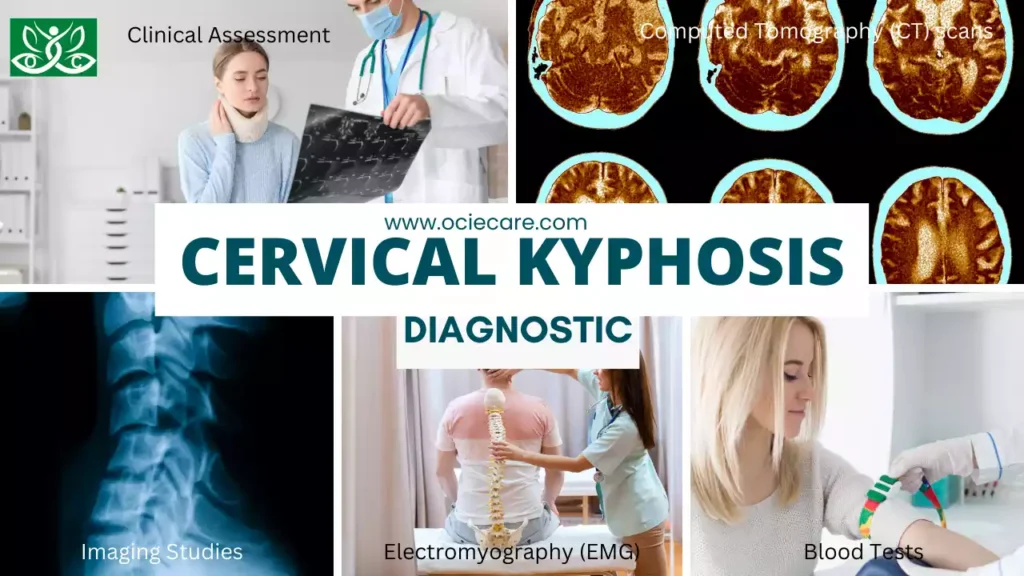
Diagnosing cervical kyphosis typically involves a comprehensive approach that includes clinical assessment, imaging studies, and sometimes laboratory tests:
1. Clinical Assessment:
This involves a thorough physical examination by a healthcare provider. They will assess the patient’s posture, neck range of motion, and look for any signs of discomfort or neurological symptoms such as numbness, tingling, or muscle weakness in the arms and hands. Clinical assessment helps in understanding the physical impact of cervical kyphosis on the patient.
A. Normal parameters of the cervical spine:
I. The normal curvature of the cervical spine should maintain a gentle inward curve, known as lordosis:
- The cervical spine, which is the upper portion of the spine located in the neck, typically exhibits a natural curve that faces inward towards the front of the body.
- This curve is known as “lordosis.” It allows the spine to distribute weight evenly and maintain stability while also providing flexibility for movements of the neck.
- When viewing the spine from the side, this inward curvature should be visibly present and not excessively flattened or reversed.
- An abnormal loss or reversal of this lordotic curve can indicate a cervical spine issue, such as cervical kyphosis.
II. Physiological range of motion in the neck without pain or stiffness:
- In a healthy individual, the cervical spine allows for a wide range of motion in the neck region.
- This means that one should be able to move the head and neck comfortably in various directions, including forward, backward, side-to-side, and rotational movements.
- Moreover, these movements should occur without any significant discomfort, pain, or stiffness.
- Normal neck function allows for activities such as turning the head to look around, tilting the head, and nodding without limitations or discomfort.
- Any restrictions in range of motion or the presence of pain and stiffness can be indicative of cervical spine issues, which should be evaluated by a healthcare professional to determine the cause and appropriate treatment.
B. Abnormal parameters associated with cervical kyphosis:
I. Excessive forward curvature of the cervical spine, leading to a “hunchback” appearance:
- Abnormal cervical kyphosis is characterized by an exaggerated forward curvature of the cervical spine.
- In this condition, the neck assumes a posture that resembles a “hunchback,” where the natural inward curve (lordosis) becomes more pronounced, leading to an abnormal forward bending of the neck.
- This altered alignment can visibly affect a person’s posture and may result in a noticeable forward-leaning or stooped appearance.
II. Limited range of motion in the neck, with pain and stiffness:
- Individuals with cervical kyphosis often experience limitations in the range of motion of their neck.
- This means they may have difficulty moving their head and neck in various directions, such as turning it from side to side, tilting it forward and backward, or rotating it.
- These restrictions in movement can be accompanied by discomfort, pain, and stiffness in the neck region.
- Such symptoms can significantly impact daily activities and quality of life.
III. Neurological symptoms like numbness, tingling, or weakness in the arms and hands due to nerve compression:
- Cervical kyphosis can lead to compression or impingement of the spinal cord or nerve roots in the neck region.
- When this occurs, individuals may experience neurological symptoms in their upper extremities.
- These symptoms can include numbness (loss of sensation), tingling sensations (paresthesia), or weakness in the arms and hands.
- The severity of these symptoms may vary depending on the degree of nerve compression and the specific nerves affected.
- If left untreated, chronic nerve compression can lead to muscle weakness and atrophy.
Summary:
Cervical kyphosis presents with several abnormal parameters, including an exaggerated forward curvature of the neck (hunchback appearance), restricted neck movement accompanied by pain and stiffness, and neurological symptoms in the arms and hands due to nerve compression. These manifestations highlight the functional and structural consequences of this spinal condition, underscoring the importance of timely diagnosis and appropriate management.
2. Imaging Studies:
These are crucial for confirming the diagnosis and understanding the extent of the condition. The most common imaging studies include X-rays and Magnetic Resonance Imaging (MRI). X-rays provide detailed images of the cervical spine’s curvature and alignment, helping to measure the degree of abnormality. MRI, on the other hand, provides more comprehensive images that allow healthcare providers to assess the soft tissues, spinal cord, and nerve roots for any compression or damage.
A. X-rays of the cervical spine to assess the degree of curvature and alignment:
- X-rays are often the initial imaging study used to evaluate cervical kyphosis.
- They provide detailed images of the bones in the cervical spine.
- Healthcare providers can use these X-rays to assess the degree of abnormal curvature and alignment of the vertebrae.
- This diagnostic tool helps quantify the extent of the kyphotic deformity and serves as a baseline for monitoring changes over time.
- X-rays are particularly valuable for assessing structural abnormalities, such as bone spurs or fractures, which may contribute to the condition.
B. Magnetic Resonance Imaging (MRI) to visualize soft tissues, spinal cord, and nerve roots:
- Magnetic Resonance Imaging (MRI) is a powerful diagnostic tool that provides detailed images of soft tissues in the neck, including muscles, ligaments, discs, the spinal cord, and nerve roots.
- This imaging modality helps identify the presence of any compression or impingement on the spinal cord or nerves.
- MRI is especially valuable for assessing the impact of cervical kyphosis on the surrounding soft tissues and for detecting conditions like disc herniation or spinal stenosis, which can contribute to symptoms.
C. Physical examination to evaluate posture, range of motion, and neurological function:
- A thorough physical examination is a crucial component of diagnosing cervical kyphosis.
- During this examination, a healthcare provider assesses the patient’s posture, looking for any visible signs of abnormal curvature or a “hunchback” appearance.
- They also evaluate the range of motion in the neck, checking for limitations, pain, or stiffness during movements like bending, turning, and tilting the head.
- Additionally, the physical examination includes a neurological assessment to evaluate nerve function.
- This may involve testing muscle strength, sensation, and reflexes in the arms and hands.
- The presence of neurological symptoms such as numbness, tingling, or weakness in the upper extremities can be indicative of nerve compression related to cervical kyphosis.
Summary:
The diagnostic process for cervical kyphosis typically involves a combination of common tests, including X-rays to assess bone structure and alignment, MRI to visualize soft tissues and assess spinal cord and nerve root compression, and a thorough physical examination to evaluate posture, range of motion, and neurological function. These diagnostic tools help healthcare providers accurately diagnose the condition, determine its severity, and develop an appropriate treatment plan tailored to the individual’s needs.
3. Specialized Diagnostic Test
Let’s delve into the specialized diagnostic tests used for cervical kyphosis:
A. Computed Tomography (CT) scans may be used to assess bony structures and the severity of spinal deformity:
- Computed Tomography (CT) scans are advanced imaging studies that provide detailed cross-sectional images of the cervical spine.
- They are particularly valuable for assessing bony structures, including the vertebrae and any abnormalities, such as bone spurs, fractures, or areas of increased bone density.
- CT scans offer a high level of precision in evaluating the severity of spinal deformities, including cervical kyphosis.
- They can provide more detailed information about the three-dimensional structure of the spine, helping healthcare providers plan surgical interventions when necessary.
CT scans are often used when there is a need for a comprehensive assessment of the bony components of cervical kyphosis, especially in cases where surgery is being considered or when there is a suspected bony abnormality contributing to the condition.
B. Electromyography (EMG) to evaluate nerve function and identify specific areas of nerve compression:
Electromyography (EMG) is a specialized test used to assess the electrical activity of muscles and the functioning of nerves. In the context of cervical kyphosis, EMG can be particularly helpful in evaluating nerve function and identifying specific areas of nerve compression or damage. Here’s how it works:
I. Needle Electrodes:
- During an EMG, fine needle electrodes are inserted into specific muscles in the arms or hands, depending on the symptoms and suspected nerve involvement.
II. Muscle Response:
- The electrical activity in the muscles is measured as the patient performs controlled muscle contractions. This helps identify abnormal electrical patterns that may be indicative of nerve dysfunction.
III. Nerve Conduction Study:
- Often combined with EMG, a nerve conduction study involves applying small electrical impulses to the nerves and measuring the speed and strength of the nerve’s response. Slower or weaker responses can indicate nerve compression or damage.
EMG is valuable for pinpointing the location and extent of nerve involvement, helping healthcare providers determine the cause of symptoms such as numbness, tingling, or weakness in the arms and hands. It can aid in identifying whether nerve compression is related to cervical kyphosis or other conditions.
Summary:
Specialized tests in the diagnosis of cervical kyphosis include Computed Tomography (CT) scans, which provide detailed images of bony structures and spinal deformities, and Electromyography (EMG), which evaluates nerve function and identifies specific areas of nerve compression or damage. These tests are crucial for a more comprehensive assessment of the condition, aiding in treatment planning and ensuring that the underlying causes and associated complications are appropriately addressed.
4. Laboratory Tests:
Cervical kyphosis is primarily a structural issue affecting the alignment of the cervical spine. As such, it does not typically result in specific laboratory abnormalities on routine blood tests or standard laboratory assessments. This is because the condition itself doesn’t directly impact blood chemistry or bodily fluids in the same way that some other medical conditions might.
However, cervical kyphosis can lead to secondary complications that may be reflected in specialized laboratory tests or diagnostic studies:
I. Electromyography (EMG):
- EMG is a specialized test used to assess the functioning of muscles and nerves.
- While cervical kyphosis itself doesn’t produce laboratory abnormalities, the condition can cause nerve compression or impingement due to the abnormal curvature of the spine.
- Nerves affected by compression may exhibit abnormal electrical activity during an EMG, indicating nerve dysfunction.
II. Nerve Conduction Studies:
- Often performed alongside EMG, nerve conduction studies evaluate the speed and strength of nerve signals.
- If cervical kyphosis is causing nerve compression, these studies may reveal reduced or delayed nerve conduction, which can be indicative of nerve damage or dysfunction.
III. Blood Tests:
- In cases where cervical kyphosis has led to secondary complications, such as muscle weakness or atrophy, blood tests may be performed to assess markers of muscle damage or inflammation.
- Elevated levels of certain enzymes in the blood, such as creatine kinase (CK) or aldolase, can indicate muscle injury.
- While these tests are not specific to cervical kyphosis, they can help diagnose and monitor complications related to the condition.
Summary:
Cervical kyphosis itself does not typically produce specific laboratory abnormalities in routine blood tests. However, the condition can lead to secondary complications, such as nerve compression or muscle weakness, which may be detected through specialized diagnostic tests like EMG, nerve conduction studies, or specific blood tests for muscle-related markers. These laboratory findings can aid in the diagnosis and management of complications associated with cervical kyphosis, ensuring that appropriate treatment measures are implemented.
Overall, cervical kyphosis is a condition characterized by an atypical forward curvature of the cervical spine, which can have a range of clinical manifestations. Diagnosis involves a combination of clinical assessment, imaging studies, and, if necessary, specialized laboratory tests. These diagnostic approaches are essential for understanding the severity of the condition and guiding appropriate treatment decisions to alleviate symptoms and improve the patient’s quality of life.
Cervical Kyphosis Treatment

The choice of treatment for cervical kyphosis is influenced by several factors, including the severity of the condition, its underlying causes, and the presence of neurological deficits.
Here are the primary treatment options:
A. Conservative Management:
I. Physical Therapy:
- Physical therapy plays a significant role in the conservative management of cervical kyphosis, particularly for mild cases.
- Therapists work with patients to improve posture, strengthen the neck and upper back muscles, and enhance flexibility.
- Specific exercises and stretches are tailored to the individual to help correct abnormal spinal curvature and alleviate associated discomfort.
II. Posture Correction:
- Education on proper posture and ergonomics is crucial.
- Patients learn how to maintain correct neck and spine alignment during daily activities, including sitting at a computer, reading, and sleeping.
- This can help prevent further progression of the kyphotic deformity.
III. Pain Management:
- Over-the-counter pain relievers or prescription medications may be recommended to manage pain and discomfort associated with cervical kyphosis.
- These medications can help improve the patient’s overall comfort and quality of life.
IV. Lifestyle Modifications:
- Patients may be advised to make lifestyle changes, such as avoiding activities that strain the neck and incorporating neck-friendly practices into their daily routines.
2. Bracing:
- In some cases, particularly when cervical kyphosis is detected in adolescents with growing spines, a cervical brace or orthosis may be prescribed.
- The brace is designed to support the neck and restrict excessive movement, helping to prevent further progression of the abnormal curvature.
- The effectiveness of bracing depends on the individual and the severity of the condition. Regular monitoring and adjustments may be necessary.
3. Surgery:
Surgical intervention is considered when conservative measures are inadequate, or when cervical kyphosis is severe, causing significant pain or neurological deficits. The decision for surgery is carefully made based on the specific characteristics of the condition and the patient’s overall health.
Surgical procedures aim to realign the cervical spine and stabilize it with instrumentation. The choice of surgery depends on factors such as the degree of curvature, the location of the deformity, and the underlying cause. Common surgical approaches include:
I. Anterior Cervical Discectomy and Fusion (ACDF):
- This procedure involves removing damaged discs and vertebral segments from the front of the neck and fusing adjacent vertebrae together using bone grafts and hardware (plates and screws).
II. Posterior Cervical Fusion:
- In this approach, the surgeon accesses the spine from the back of the neck to fuse the affected vertebrae, correcting the curvature.
III. Osteotomy:
- In severe cases, surgeons may perform osteotomy, which involves cutting and repositioning the vertebrae to correct the abnormal curvature.
Surgery carries certain risks, including infection, hardware failure, and changes in neck motion. The decision for surgery should be made in consultation with a spine specialist and is tailored to the individual’s unique circumstances.
Summary:
The treatment of cervical kyphosis is individualized and depends on factors such as the severity of the condition, its underlying causes, and the presence of neurological deficits. Conservative management, including physical therapy and posture correction, is often effective for mild cases. Bracing may be considered to prevent further progression. Surgery is reserved for severe cases or when neurological deficits are present and involves realigning the spine and stabilizing it with instrumentation. The choice of treatment is made in consultation with healthcare providers to ensure the best possible outcome for the patient.
Cervical Kyphosis Exercises
While home exercises cannot cure cervical kyphosis, they can help improve neck posture, strengthen supporting muscles, and alleviate some associated discomfort. It’s important to consult with a healthcare provider or physical therapist before starting any exercise regimen, especially if you have cervical spine issues.
Here are some exercises that may be recommended:
1. Chin Tucks:
- Sit or stand with your shoulders relaxed.
- Gently tuck your chin towards your chest without tilting your head up or down.
- Hold for a few seconds and then release.
- Repeat 10-15 times.
2. Neck Retraction:
- Sit or stand with good posture.
- Slowly pull your head back, as if trying to make a “double chin” without tilting your head up or down.
- Hold for a few seconds and release.
- Repeat 10-15 times.
3. Neck Stretches:
- Gently tilt your head to one side, bringing your ear towards your shoulder.
- Hold for 15-30 seconds.
- Repeat on the other side.
- You can also tilt your head forward and backward for additional stretches.
4. Neck Rotations:
- Turn your head to the right as if looking over your shoulder.
- Hold for 15-30 seconds.
- Return to the center and repeat on the left side.
5. Shoulder Blade Squeezes:
- Sit or stand with your arms at your sides.
- Squeeze your shoulder blades together, as if trying to hold a pencil between them.
- Hold for 5-10 seconds, then release.
- Repeat 10-15 times.
6. Doorway Stretch:
- Stand in a doorway with your arms at shoulder level.
- Place your palms and forearms against the door frame.
- Lean forward gently to stretch your chest and front shoulder muscles.
- Hold for 15-30 seconds.
7. Wall Angels:
- Stand with your back against a wall.
- Raise your arms to shoulder height, with your elbows bent at 90 degrees.
- Slowly slide your arms up and down the wall in a “snow angel” motion.
- This exercise helps improve shoulder and upper back mobility.
8. Posture Awareness:
- Be mindful of your posture throughout the day.
- Sit and stand with your shoulders back, chest open, and chin slightly tucked.
- Avoid prolonged periods of looking down at screens or reading materials.
Remember to perform these exercises gently and within your comfort zone. If you experience pain or discomfort while doing any exercise, stop immediately and consult a healthcare professional. Additionally, consistent exercise and good posture habits can complement other treatments for cervical kyphosis prescribed by your healthcare provider.
Cervical Kyphosis Before and After
Before and after photos or visual representations can be helpful in understanding the potential impact of treatment for cervical kyphosis. However, it’s important to note that the extent of improvement can vary widely depending on factors such as the severity of the condition, the chosen treatment approach, and the individual’s response to treatment.
A. Before Cervical Kyphosis Treatment:
- Before treatment, an individual with cervical kyphosis may exhibit noticeable signs, including an abnormal forward curvature of the neck, reduced neck mobility, and changes in posture.
- This may result in a hunched appearance of the upper back and neck.
B. After Cervical Kyphosis Treatment:
- After appropriate treatment, which may include physical therapy, bracing, or surgery, there can be improvements in the alignment of the cervical spine and overall posture.
- The extent of improvement may vary, but the goal of treatment is often to reduce pain, enhance mobility, and correct spinal alignment.
It’s crucial to consult with a healthcare provider or spine specialist to determine the most suitable treatment plan for cervical kyphosis. The effectiveness of treatment and the extent of improvement can differ from person to person, and the choice of treatment will depend on individual factors and the specific characteristics of the condition. Visual changes in posture and alignment are often part of the treatment goals, but they may vary in each case.
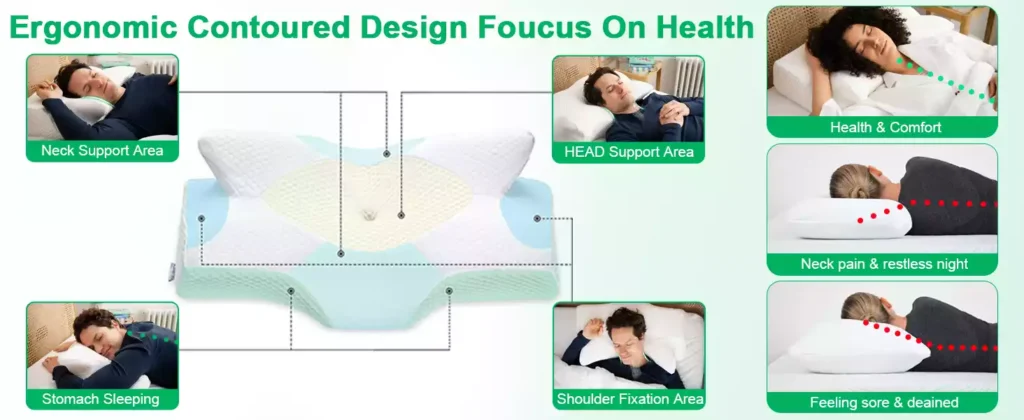
Cervical Pillow
A cervical pillow, also known as an orthopedic or contour pillow, is a specialized type of pillow designed to provide support and promote proper alignment of the cervical spine, which is the portion of the spine located in the neck. Unlike standard pillows, which are often uniform in shape and thickness, cervical pillows have a unique contour that follows the natural curve of the neck and head.
A. Key features of cervical pillows include:
I. Contoured Shape:
- Cervical pillows typically have a contour with a lower central area and raised edges. This design is intended to cradle the head and neck while providing support to maintain the natural cervical curve.
II. Different Heights:
- Cervical pillows come in various sizes and heights to accommodate different body types and sleeping positions. Individuals can choose a pillow that suits their specific needs and comfort preferences.
III. Materials:
- These pillows are made from a range of materials, including memory foam, latex, or even water-filled chambers. The choice of material can impact the firmness and comfort of the pillow.
B. The primary benefits of using a cervical pillow include:
I. Proper Alignment:
- Cervical pillows are designed to keep the head and neck in a neutral position during sleep, which can help reduce strain and promote spinal alignment.
II. Reduced Neck Pain:
- Many people find relief from neck pain, stiffness, and discomfort by using cervical pillows, especially if they have conditions like cervical kyphosis, cervical spondylosis, or herniated discs.
III. Improved Sleep Quality:
- The improved comfort and support provided by cervical pillows can lead to better sleep quality and reduced sleep disturbances.
IV. Prevention of Neck Issues:
- Cervical pillows can be used proactively to prevent neck issues from developing, particularly for individuals who spend extended hours working at a desk or looking at screens.
Summary:
It’s important to note that the effectiveness of a cervical pillow can vary from person to person. Some individuals may find significant relief and improvements in their sleep quality and neck comfort, while others may not experience the same benefits. Consulting with a healthcare provider or a specialist in spinal health can provide guidance on whether a cervical pillow is suitable for your specific needs and condition.
Cervical Pillow Amazon
1. Cervical Traction Device

The “RESTCLOUD Neck and Shoulder Relaxer” is a cervical traction device designed to provide pain relief and promote proper cervical spine alignment. Here are some key points about this Amazon product:
Purpose:
- This device is intended to alleviate various neck-related issues, including TMJ pain and discomfort associated with cervical spine misalignment.
Design:
- The RESTCLOUD Neck and Shoulder Relaxer features a contoured shape with a central depression to cradle the head and neck. Its design aims to provide gentle traction and support to the cervical spine.
Color:
- The product is available in a blue color.
Use:
- Users can lay down on the device, allowing it to support the natural curvature of the neck while promoting relaxation and tension relief.
Benefits:
- It may help reduce neck pain, stiffness, and muscle tension. By gently stretching and aligning the cervical spine, it aims to improve overall comfort.
Chiropractic Pillow:
- The product is described as a “Chiropractic Pillow Neck Stretcher,” indicating its potential alignment benefits similar to chiropractic care.
TMJ Pain Relief:
- In addition to neck pain relief, it specifically targets TMJ (temporomandibular joint) pain, which is associated with jaw discomfort.
Materials:
- The materials used in the device, such as foam or other cushioning materials, can impact its comfort and support.
Usage Recommendations:
- Users should follow the manufacturer’s recommendations for usage, including duration and frequency.
Customer Reviews:
- Rating :
4.2 out of 5 stars From 77,026 ratings - By feature:
Sturdiness : 4.8
Easy to use : 4.5
Comfort : 4.3
Support : 4.0
Pain relief : 4.0
Range of motion : 4.0
As with any health-related device, it’s advisable to consult with a healthcare provider or specialist, especially if you have specific medical conditions or concerns related to your neck and spine. This product may offer relief for some individuals, but individual experiences may vary.
2. Contour Memory Foam Pillow

The “DONAMA Cervical Pillow” is a memory foam orthopedic pillow designed to provide neck pain relief and support for various sleeping positions. Here are key points about this Amazon product:
Purpose:
- This pillow is designed to alleviate neck pain and discomfort by promoting proper spinal alignment while sleeping. It is suitable for side, back, and stomach sleepers.
Memory Foam:
- The pillow is constructed with contour memory foam, which conforms to the shape of the neck and head, providing personalized support and comfort.
Size:
- It is available in a Queen size, which is suitable for most standard bed pillows.
Color:
- The product comes in a light grey color.
Ergonomic Design:
- The pillow features an ergonomic design with contours that support the natural curvature of the cervical spine.
Breathable Pillowcase:
- Included is a breathable pillowcase that helps regulate temperature and keeps the pillow fresh.
Sleeping Positions:
- It is versatile and designed to accommodate side sleepers, back sleepers, and stomach sleepers, providing customized support for each position.
Neck Pain Relief:
- The contour memory foam and ergonomic design aim to reduce neck pain, stiffness, and tension.
Orthopedic Support:
- It is described as an orthopedic neck support pillow, indicating its focus on promoting proper neck and spine alignment.
Maintenance:
- Care and maintenance instructions should be followed to ensure the longevity of the pillow.
User Reviews:
- Rating:
4.4 out of 5 stars From 7,491 global ratings - By feature
Comfort : 4.6
Softness : 4.6
Support : 4.5
Value for money : 4.5
Sleep quality : 4.4
Pain relief : 4.3
As with any pillow designed for orthopedic support and pain relief, individual experiences may vary. It’s important to consider your specific sleep preferences and consult with a healthcare provider or specialist if you have particular neck or spine-related concerns.
3. Elviros Cervical Memory Foam Contour Pillow
The “Elviros Cervical Memory Foam Contour Pillow” is an orthopedic sleeping support pillow designed to address neck and shoulder pain. Here are key points about this Amazon product:
Purpose:
- This pillow is specifically crafted to provide ergonomic support for individuals experiencing neck and shoulder pain, making it suitable for side sleepers, back sleepers, and stomach sleepers.
Memory Foam:
- The pillow is made from memory foam, which contours to the shape of the neck and shoulders, providing customized support and comfort.
Design:
- It features a contour design that supports the natural curvature of the cervical spine, promoting proper alignment during sleep.
Sleeping Positions:
- The pillow is versatile and suitable for various sleeping positions, making it adaptable to individual preferences.
Orthopedic Support:
- It is described as an orthopedic sleeping support pillow, indicating its focus on addressing orthopedic concerns related to the neck and shoulders.
Maintenance:
- Proper care and maintenance instructions should be followed to ensure the longevity and hygiene of the pillow.
Breathable Pillowcase:
- It may include a breathable pillowcase that helps regulate temperature and maintain freshness.
User Reviews:
- Rating:
3.9 out of 5 From 44,508 global ratings - By feature
Support : 3.7
Softness : 3.6
Comfort : 3.5
Sleep quality : 3.5
Pain relief : 3.4
For traveling : 2.8
Individual experiences with orthopedic pillows can vary, so it’s important to consider your specific needs and consult with a healthcare provider if you have particular concerns related to neck and shoulder pain or sleep posture.
Conclusion
In conclusion, cervical kyphosis is a spinal condition characterized by an abnormal forward curvature of the cervical spine. This condition can have various underlying causes, including congenital factors, degenerative changes, poor posture, traumatic injuries, or neuromuscular conditions.
The symptoms of cervical kyphosis can range from neck pain and stiffness to neurological symptoms such as numbness, tingling, and weakness in the arms and hands. Changes in posture, muscle weakness, and difficulty with balance may also be present.
Diagnosis typically involves a combination of clinical assessment, imaging studies (X-rays, MRI, CT scans), and specialized tests like electromyography (EMG) to evaluate nerve function.
Treatment approaches are individualized based on the severity of the condition and its underlying causes. Conservative management, including physical therapy and bracing, may be effective for mild cases, while surgery is reserved for severe cases or when neurological deficits are present.
Timely diagnosis and appropriate treatment are essential to manage symptoms, prevent further progression, and improve the patient’s overall quality of life. With the right approach, many individuals with cervical kyphosis can find relief, regain mobility, and lead fulfilling lives.
FAQs
Q. What is cervical kyphosis?
A. Cervical kyphosis is a spinal condition characterized by an abnormal forward curvature of the cervical spine, which is the uppermost part of the spine located in the neck region.
Q. What causes cervical kyphosis?
A. Cervical kyphosis can have various underlying causes, including congenital factors, degenerative changes, poor posture, traumatic injuries, or neuromuscular conditions.
Q. What are the common symptoms of cervical kyphosis?
A. Common symptoms may include neck pain and stiffness, reduced neck mobility, headaches, numbness, tingling, or weakness in the arms and hands (due to nerve compression), muscle weakness or atrophy, changes in posture (hunchback appearance), and difficulty with balance and coordination.
Q. How is cervical kyphosis diagnosed?
A. Diagnosis typically involves a combination of clinical assessment, imaging studies (X-rays, MRI, CT scans), and specialized tests like electromyography (EMG) to evaluate nerve function.
Q. Can cervical kyphosis be treated without surgery?
A. Yes, in mild cases, conservative management may be effective. This can include physical therapy, posture correction, pain management, and bracing. The treatment approach depends on the severity and underlying causes.
Q. When is surgery recommended for cervical kyphosis?
A. Surgery is typically considered for severe cases or when neurological deficits are present. Surgical procedures aim to realign the spine and stabilize it with instrumentation.
Q. Is cervical kyphosis a congenital condition?
A. It can be congenital, meaning some individuals are born with structural abnormalities that predispose them to cervical kyphosis. However, it can also develop later in life due to other causes.
Q. Can cervical kyphosis be prevented?
A. Preventing cervical kyphosis may involve maintaining good posture, especially when using electronic devices for extended periods. Early intervention for conditions that can lead to kyphosis, such as degenerative changes, can also help prevent its development.
Q. What is the prognosis for individuals with cervical kyphosis?
A. The prognosis varies depending on factors such as the underlying cause, the severity of the curvature, and the success of treatment. Early diagnosis and appropriate management can often prevent symptom progression and improve quality of life.
Q. Can cervical kyphosis lead to long-term complications?
A. Yes, if left untreated, cervical kyphosis can lead to long-term complications, including chronic pain, nerve damage, muscle weakness, and changes in spinal alignment. Timely treatment is essential to mitigate these risks.
You may also like:
- Pelvic Organ Prolapse | Natural Treatment Without Medicine In 2023
2. Blood Sugar | Diabetes: Understanding, Treatment, and Prevention In 2023

I don’t think the title of your article matches the content lol. Just kidding, mainly because I had some doubts after reading the article.