Pelvic organ prolapse is a condition that affects many women worldwide. It occurs when the pelvic organs, such as the bladder, uterus, or rectum, descend or bulge into the vaginal canal. This article aims to provide a comprehensive overview of pelvic organ prolapse, its causes, symptoms, and various treatment options, including natural solutions.

Pelvic Organ Prolapse: Natural Treatment Without Medicine In 2023
Introduction: What is Pelvic Organ Prolapse?
Pelvic organ prolapse occurs when the muscles and tissues that support the pelvic organs become weakened or damaged, leading to their descent or bulging into the vaginal canal. This condition often results from childbirth, menopause, obesity, chronic coughing, or heavy lifting.
Causes and Risk Factors Pelvic Organ Prolapse
The primary cause of pelvic organ prolapse is weakened or stretched pelvic floor muscles and ligaments. These supportive structures play a crucial role in maintaining the position and stability of the pelvic organs. When they become weakened or damaged, it can lead to the descent or bulging of the pelvic organs into the vaginal canal.
Let’s delve deeper into the factors that increase the risk of developing pelvic organ prolapse:
I. Vaginal childbirth:
The process of giving birth vaginally can exert significant pressure on the pelvic floor muscles and tissues. The stretching and strain during childbirth can weaken these structures, making them more susceptible to prolapse later in life. Women who have undergone multiple childbirths or experienced prolonged pushing during delivery are at a higher risk.
II. Aging and menopause:
As women age, the levels of estrogen, a hormone that helps maintain the strength and elasticity of the pelvic floor muscles and tissues, decrease. This hormonal change can contribute to the weakening of these structures, increasing the likelihood of prolapse. Additionally, the natural aging process can lead to the loss of muscle tone and the deterioration of connective tissues in the pelvic region.
III. Chronic constipation or straining during bowel movements:
Frequent constipation or the habit of straining during bowel movements puts excessive pressure on the pelvic floor. This repeated strain can weaken the muscles and ligaments over time, making them more prone to prolapse.
IV. Obesity:
Excess weight and obesity can put additional strain on the pelvic floor muscles and tissues. The increased pressure from carrying extra weight can contribute to their weakening and subsequent prolapse. Maintaining a healthy weight is important in reducing the risk of developing pelvic organ prolapse.
V. Genetic predisposition:
Some individuals may have a genetic predisposition to pelvic organ prolapse. Certain genetic factors can influence the strength and integrity of the pelvic floor structures, making some people more susceptible to prolapse than others. However, it’s important to note that genetic predisposition alone is not the sole cause of prolapse, and other factors often contribute to its development.
VI. Chronic coughing or conditions that put pressure on the pelvic area:
Chronic coughing due to conditions like asthma, bronchitis, or long-term smoking can lead to increased abdominal pressure. This constant pressure can weaken the pelvic floor muscles and ligaments, making prolapse more likely. Similarly, conditions that cause chronic strain on the pelvic area, such as heavy lifting or repetitive high-impact activities, can also contribute to the development of prolapse.
It’s essential to recognize that while these factors increase the risk of pelvic organ prolapse, not everyone who experiences them will develop the condition. Additionally, some individuals may develop prolapse without any identifiable risk factors. It’s a multifactorial condition influenced by a combination of factors, and each person’s experience may vary.
Understanding the causes and risk factors of pelvic organ prolapse helps individuals and healthcare professionals take preventive measures and develop appropriate treatment plans. By addressing these underlying factors, it is possible to reduce the risk of developing or worsening pelvic organ prolapse and improve overall pelvic floor health.
Types of Pelvic Organ Prolapse
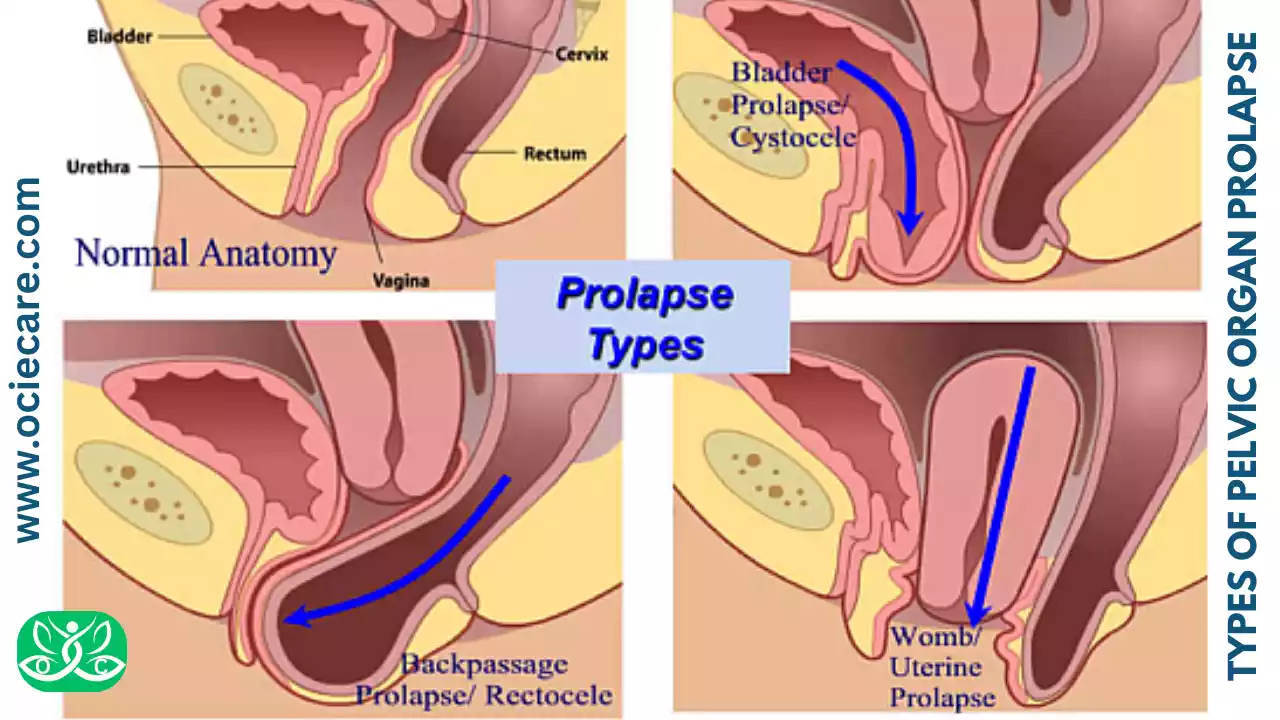
Pelvic organ prolapse can involve different organs within the pelvic region. Depending on which organ is affected, specific types of prolapse can occur. Here are the four main types of pelvic organ prolapse:
I. Cystocele:
A cystocele refers to the descent of the bladder into the vagina. The bladder is located in the pelvic area, just above the vagina. In a cystocele, the supportive tissues between the bladder and the vaginal wall weaken, causing the bladder to sag or bulge into the vaginal space. This can lead to symptoms such as a feeling of pelvic pressure, discomfort during sexual intercourse, urinary leakage, frequent urinary tract infections, or difficulty fully emptying the bladder.
II. Rectocele:
A rectocele occurs when the rectum, which is located behind the vagina, protrudes into the vaginal space. Weakness in the tissues separating the rectum and the vagina allows the rectum to bulge or herniate into the vaginal wall. Symptoms of a rectocele may include difficulty with bowel movements, a sensation of incomplete emptying, the need to use manual pressure on the vagina or perineum to facilitate bowel movements, and a feeling of rectal fullness.
III. Uterine prolapse:
Uterine prolapse refers to the descent of the uterus into the vaginal canal. The uterus is held in place by supportive ligaments and muscles. When these structures weaken or stretch, the uterus can descend and protrude into the vaginal space. Uterine prolapse may cause symptoms such as a sensation of pelvic pressure or heaviness, lower back pain, difficulty with sexual intercourse, urinary incontinence, or problems with bowel movements.
IV. Vaginal vault prolapse:
Vaginal vault prolapse occurs when the top part of the vagina descends or protrudes into the lower vagina or even outside the vaginal opening. This type of prolapse typically occurs in women who have had a hysterectomy (removal of the uterus). After the uterus is removed, the top portion of the vagina, known as the vaginal vault, can lose support and sag. Symptoms may include a noticeable bulge or pressure in the vaginal area, discomfort or pain during intercourse, or difficulty inserting tampons.
It’s important to note that pelvic organ prolapse can involve more than one type simultaneously, and the severity of prolapse can vary among individuals. Healthcare professionals specializing in pelvic floor disorders can perform a thorough examination to identify the specific types of prolapse and recommend appropriate treatment options based on individual circumstances.
The treatment for pelvic organ prolapse may involve a combination of lifestyle modifications, pelvic floor exercises, the use of supportive devices such as pessaries, or surgical interventions. Consulting with a healthcare professional is crucial to determine the most suitable treatment plan tailored to your specific needs and symptoms.
Yeast Infection: 5 Steps Natural Solutions Within 12 Hrs.
Pelvic Organ Prolapse Stages
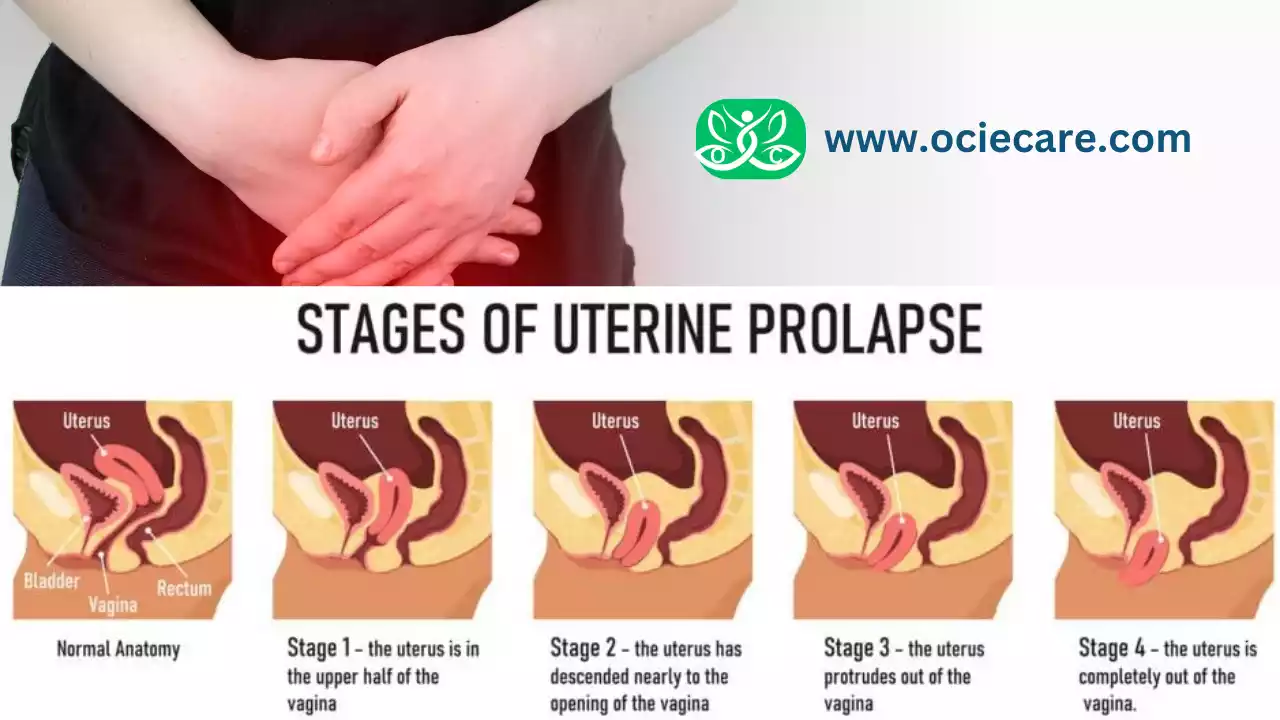
Pelvic organ prolapse can be categorized into different stages based on the severity and extent of the descent or bulging of the pelvic organs. The staging system helps healthcare professionals assess and communicate the degree of prolapse. Although different staging systems exist, the most commonly used classification is the Baden-Walker System. Let’s explore the stages of pelvic organ prolapse in more detail:
I. Stage 0 (No prolapse):
In this stage, there is no descent or bulging of the pelvic organs. The pelvic organs are well supported, and there are no noticeable symptoms or physical changes.
II. Stage I (Mild prolapse):
In stage, I, the descent of the pelvic organs is minimal and occurs only within the upper two-thirds of the vagina. This stage is often characterized by subtle changes, such as a feeling of pelvic pressure or discomfort, particularly during physical exertion.
III. Stage II (Moderate prolapse):
Stage II prolapse involves a more significant descent of the pelvic organs, extending beyond the upper two-thirds of the vagina but not reaching the vaginal opening. At this stage, the prolapse may be noticeable as a bulge or protrusion felt within the vagina. Symptoms may include a sense of heaviness or pressure in the pelvic region, discomfort during intercourse, and urinary or bowel symptoms.
IV. Stage III (Advanced prolapse):
Stage III prolapse is characterized by a substantial descent of the pelvic organs, with the prolapse reaching the vaginal opening or even protruding outside the vaginal opening. The symptoms become more pronounced, and the protrusion may be visible or palpable outside the body. It can cause significant discomfort, difficulties with urinary and bowel function, and sexual limitations.
V. Stage IV (Complete prolapse):
Stage IV prolapse is the most severe stage, with the pelvic organs fully descending and protruding outside the vaginal opening. The prolapse may be visible without the need for internal examination. This stage can lead to significant functional impairment and impact daily activities, causing discomfort, difficulty with urinary and bowel control, and challenges with sexual intercourse.
It’s important to note that the symptoms and impact on daily life may not always correlate directly with the stage of prolapse. Some individuals with milder prolapse may experience significant symptoms, while others with advanced prolapse may have minimal symptoms. The staging system serves as a guide for healthcare professionals to understand the anatomical extent of prolapse, but it is not the sole determinant of treatment decisions. Each person’s experience is unique, and the treatment plan should be tailored to their specific symptoms, goals, and overall health.
If you suspect or have been diagnosed with pelvic organ prolapse, consulting with a healthcare professional specializing in pelvic floor disorders will help determine the appropriate management and treatment options based on your circumstances.
Common Symptoms of Pelvic Organ Prolapse
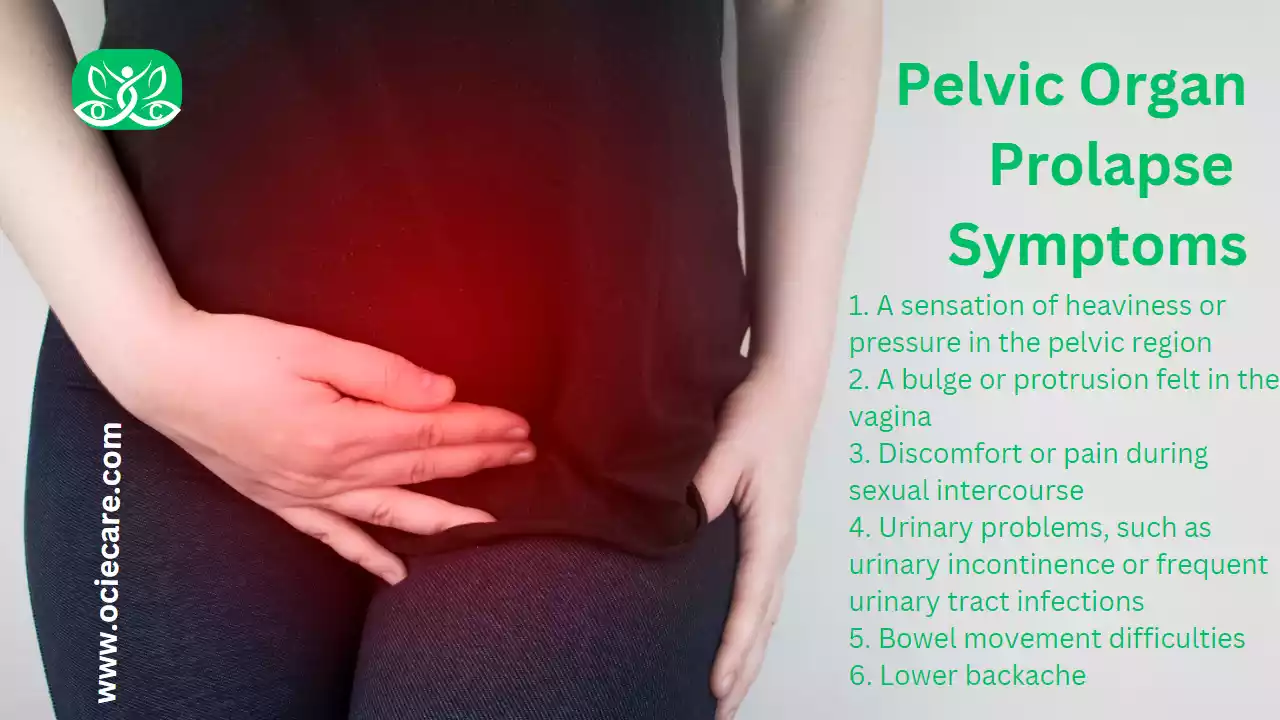
Pelvic organ prolapse can manifest in various ways, and the symptoms experienced by individuals may differ based on the severity and type of prolapse. Understanding these common symptoms can help in recognizing and seeking appropriate medical attention.
Here are some elaborations, explanations, and examples for better understanding:
I. A sensation of heaviness or pressure in the pelvic region:
Many individuals with pelvic organ prolapse describe a persistent feeling of heaviness or pressure in the lower abdominal or pelvic area. It can be likened to a dragging or pulling sensation and is often more pronounced after prolonged standing or physical exertion. Imagine carrying a heavy object in your pelvis, causing discomfort and a constant awareness of pressure.
II. A bulge or protrusion felt in the vagina:
One of the hallmark signs of pelvic organ prolapse is the presence of a bulge or protrusion felt within the vaginal canal. This bulge may vary in size and shape depending on the specific organ involved. For example, in the case of cystocele (bladder prolapse), a bulge at the front of the vaginal wall may be noticeable. The sensation of a bulge can be similar to that of a small grape or a soft lump.
III. Discomfort or pain during sexual intercourse:
Pelvic organ prolapse can lead to discomfort or pain during sexual intercourse, known as dyspareunia. The descent of the pelvic organs can alter the position and shape of the vaginal canal, causing friction or pressure during penetration. This can result in physical discomfort and a decrease in sexual satisfaction or desire.
IV. Urinary problems, such as urinary incontinence or frequent urinary tract infections:
Prolapse can affect the proper functioning of the urinary system. Some individuals may experience urinary incontinence, which involves the involuntary leakage of urine, particularly during activities that increase intra-abdominal pressure, such as coughing, sneezing, or lifting heavy objects. Others may develop recurrent urinary tract infections due to compromised anatomical support and impaired bladder emptying associated with prolapse.
V. Bowel movement difficulties:
Pelvic organ prolapse can interfere with normal bowel movements. Individuals may experience difficulty in fully emptying their bowels or have a sense of incomplete evacuation. This can result from changes in the anatomical alignment and pressure on the rectum caused by rectocele (rectal prolapse). Straining during bowel movements may become necessary, leading to constipation and further aggravation of pelvic floor dysfunction.
VI. Lower backache:
Pelvic organ prolapse can cause lower back pain due to the altered position and support of the pelvic organs. The strain on the pelvic floor muscles and ligaments can lead to muscular imbalances and increased pressure on the lower back, resulting in persistent discomfort or dull aches in that region.
It’s important to note that these symptoms can vary in severity and may not all be present simultaneously. Some individuals may experience mild symptoms that don’t significantly impact their daily lives, while others may have more pronounced symptoms that affect their overall well-being. If you are experiencing any of these symptoms, it is recommended to consult with a healthcare professional for proper evaluation and management.
Remember, early detection and appropriate treatment can help alleviate symptoms and improve the quality of life for individuals with pelvic organ prolapse.
Pelvic Organ Prolapse (POP) and Leaking
Pelvic organ prolapse (POP) and leaking, specifically urinary incontinence, can often coexist and be interconnected. Pelvic organ prolapse refers to the descent or bulging of the pelvic organs, such as the bladder, uterus, or rectum, into the vaginal canal or outside the body. This descent can put pressure on the urethra, the tube that carries urine from the bladder, and contribute to urinary incontinence.
Different types of urinary incontinence may be associated with pelvic organ prolapse:
I. Stress incontinence:
This is the most common type of incontinence seen in women with pelvic organ prolapse. It occurs when there is leakage of urine during activities that increase intra-abdominal pressure, such as coughing, sneezing, laughing, or lifting heavy objects. The weakened pelvic floor muscles and compromised support of the bladder and urethra in pelvic organ prolapse contribute to stress incontinence.
II. Urge incontinence:
In some cases, pelvic organ prolapse can also cause urge incontinence, which is characterized by a sudden and strong urge to urinate followed by involuntary urine leakage. The prolapse may irritate the bladder or disrupt its normal function, leading to the frequent and urgent need to urinate.
III. Mixed incontinence:
Mixed incontinence refers to a combination of stress and urge incontinence. Women with pelvic organ prolapse may experience both types of incontinence simultaneously, with leakage occurring during physical activities as well as in response to an urge to urinate.
It is important to note that not all women with pelvic organ prolapse will experience urinary incontinence. The severity of the prolapse, the degree of muscle weakness, and individual factors can influence the presence and severity of leakage.
Treatment options for urinary incontinence associated with pelvic organ prolapse may include:
I. Pelvic floor muscle exercises:
Strengthening the pelvic floor muscles through exercises such as Kegels can help improve muscle tone and support the bladder and urethra, reducing urinary leakage.
II. Lifestyle modifications:
Maintaining a healthy weight, avoiding constipation, managing chronic coughing, and limiting caffeine and alcohol intake can all contribute to better bladder control and reduce urinary incontinence.
III. Bladder training:
Learning techniques to gradually increase the time between bathroom visits and control the urge to urinate can help manage urge incontinence associated with pelvic organ prolapse.
IV. Pessaries:
A pessary, a device inserted into the vagina to support the pelvic organs, can help alleviate both pelvic organ prolapse and urinary incontinence symptoms by reducing pressure on the bladder and urethra.
V. Surgery:
In severe cases or when conservative measures are not effective, surgical intervention may be recommended to repair the prolapse and address urinary incontinence.
It is essential to consult with a healthcare professional, such as a gynecologist or urogynecologist, for an accurate diagnosis and to develop an appropriate treatment plan based on your specific symptoms and circumstances. They can evaluate the extent of the prolapse, assess the severity of urinary incontinence, and recommend the most suitable treatment options for you.
Become a Home Doctor: Learn to be Self-Reliant & Self-Care In 2023
Diagnosing Pelvic Organ Prolapse

Diagnosing pelvic organ prolapse involves a thorough evaluation that combines a physical examination and a detailed medical history. Additional tests may also be conducted to assess the severity of the condition and its impact on the pelvic organs. Here’s a more detailed explanation of the diagnostic process:
I. Physical examination:
The first step in diagnosing pelvic organ prolapse is a physical examination performed by a healthcare professional. During this examination, the doctor will visually inspect the pelvic area and may ask you to bear down or cough to assess the descent of the pelvic organs. The doctor will also perform a pelvic floor muscle assessment to evaluate the strength and tone of the pelvic floor muscles.
II. Medical history:
A detailed medical history is crucial in understanding the symptoms, duration, and impact of the condition on your daily life. The doctor will inquire about any symptoms you are experiencing, such as pelvic pressure, vaginal bulging, or urinary and bowel problems. They will also ask about your medical and surgical history, pregnancies and deliveries, menopausal status, and any relevant factors that may contribute to the development of pelvic organ prolapse.
III. Urodynamic testing:
In some cases, urodynamic testing may be recommended to assess bladder function and identify any associated urinary problems. Urodynamic tests evaluate how the bladder and urethra are functioning during filling and emptying. These tests can help determine if urinary incontinence or other bladder dysfunctions are present alongside pelvic organ prolapse.
IV. Imaging studies:
Imaging studies such as pelvic ultrasound or magnetic resonance imaging (MRI) may be ordered to obtain more detailed information about the pelvic organs and their position. These imaging techniques can provide visual confirmation of prolapse and help determine the severity and extent of the condition. They can also help identify any other abnormalities or conditions that may be contributing to the symptoms.
The combination of physical examination, medical history, and additional tests allows healthcare professionals to accurately diagnose pelvic organ prolapse and understand its impact on an individual’s pelvic floor health. It also helps in developing an appropriate treatment plan tailored to the specific needs of the patient.
If you are experiencing symptoms suggestive of pelvic organ prolapse, it is important to consult with a healthcare professional who specializes in pelvic floor disorders. They will be able to conduct a comprehensive evaluation and provide the necessary guidance and treatment options to address your condition effectively.
Conventional Treatment Options Pelvic Organ Prolapse
The treatment of pelvic organ prolapse is determined by the severity of symptoms and the impact on a person’s quality of life. Here are some conventional treatment options commonly used for managing pelvic organ prolapse:
A. Lifestyle Modifications:
Making certain lifestyle changes can help alleviate pelvic organ prolapse symptoms and prevent further progression. These modifications may include:
I. Maintaining a healthy weight:
Excess weight can strain the pelvic floor muscles and exacerbate prolapse symptoms. Maintaining a healthy weight through a balanced diet and regular exercise can reduce the burden on the pelvic floor and provide better support for the pelvic organs.
II. Avoiding heavy lifting:
Engaging in heavy lifting activities can increase intra-abdominal pressure, putting stress on the weakened pelvic floor. Minimizing heavy lifting or using proper lifting techniques can help prevent further strain on the pelvic floor muscles.
III. Managing chronic coughing:
Chronic coughing, such as that caused by smoking or respiratory conditions, can contribute to prolapse. Managing and treating chronic coughing effectively, such as through medication or lifestyle changes, can help reduce the strain on the pelvic floor.
IV. Incorporating dietary modifications:
Maintaining regular bowel movements and preventing constipation can reduce strain during bowel movements. Eating a high-fiber diet, staying hydrated, and avoiding constipation-triggering foods can help promote regularity and prevent excessive straining.
B. Pelvic Floor Exercises:
Pelvic floor muscle exercises, commonly known as Kegel exercises, are a key component of pelvic organ prolapse management. These exercises involve contracting and relaxing the muscles that support the pelvic organs. Regular and proper performance of pelvic floor exercises can strengthen the pelvic floor muscles, improve support for the organs, and alleviate prolapse symptoms. Physical therapists specializing in pelvic floor health can guide you in performing these exercises correctly.
C. Pessaries:
A pessary is a removable device that is inserted into the vagina to provide support for the prolapsed organs. Pessaries come in various shapes and sizes and are fitted by healthcare professionals based on an individual’s specific needs. They work by mechanically supporting the pelvic organs and reducing the symptoms of prolapse. Pessaries can be an effective non-surgical option for managing pelvic organ prolapse, particularly for individuals who wish to avoid or delay surgery.
D. Surgical Interventions:
In severe cases where conservative measures are ineffective or when prolapse significantly affects a person’s quality of life, surgical intervention may be recommended. Surgical procedures for pelvic organ prolapse aim to repair and restore the pelvic floor structures, providing better support for the organs. The specific surgical approach depends on various factors, such as the type and severity of prolapse, individual circumstances, and surgeon expertise. Surgical interventions can be performed through the vagina or using minimally invasive techniques, such as laparoscopic or robotic-assisted surgery.
It’s important to note that the choice of treatment depends on individual factors, including the severity of prolapse, overall health, personal preferences, and desired outcomes. Consulting with a healthcare professional who specializes in pelvic floor disorders will help determine the most appropriate treatment plan tailored to your specific needs and goals.
Natural Solutions for Pelvic Organ Prolapse
In addition to conventional treatments, several natural solutions can be considered to alleviate symptoms and support the overall well-being of individuals with pelvic organ prolapse. These natural approaches focus on strengthening the pelvic floor muscles, promoting a healthy lifestyle, exploring herbal remedies, and incorporating alternative therapies. Here are further details and explanations:
A. Pelvic Floor Muscle Training:
Similar to conventional pelvic floor exercises, specialized training programs, and physical therapy can help strengthen the pelvic floor muscles and improve symptoms of prolapse. These programs may include specific exercises targeting the pelvic floor muscles, such as Kegel exercises, as well as techniques to improve muscle coordination and awareness. Pelvic floor muscle training aims to enhance the strength and endurance of the muscles, providing better support for the pelvic organs and reducing prolapse symptoms.
B. Healthy Lifestyle Practices:
Maintaining a healthy lifestyle can positively impact pelvic floor health and potentially slow down the progression of pelvic organ prolapse. Some healthy lifestyle practices include:
I. Regular exercise:
Engaging in regular physical activity, such as walking, swimming, or low-impact exercises, can help strengthen overall muscle tone, including the pelvic floor muscles. It is important to choose exercises that are safe and appropriate for individual circumstances.
II. Balanced diet:
Consuming a nutritious, well-balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall tissue health and provide essential nutrients for muscle function. Adequate hydration is also crucial to maintain optimal tissue elasticity.
III. Maintaining a healthy weight:
Excess weight can place additional strain on the pelvic floor muscles and worsen prolapse symptoms. Maintaining a healthy weight through a combination of regular exercise and a balanced diet can help reduce the burden on the pelvic floor and support its proper function.
C. Herbal Remedies:
Some herbal remedies are believed to have beneficial effects on pelvic organ prolapse symptoms. However, it is important to note that scientific evidence regarding the effectiveness and safety of these remedies is limited. Examples of herbal remedies that are sometimes used include:
I. Horse chestnut:
Horse chestnut extract has been traditionally used to promote blood vessel health and reduce swelling. It is believed to have potential benefits in managing pelvic organ prolapse symptoms, although more research is needed to establish its efficacy.
II. Red raspberry leaf:
Red raspberry leaf is commonly used in traditional medicine for its potential benefits on the female reproductive system. It is believed to support uterine and pelvic floor health. However, scientific evidence supporting its effectiveness for pelvic organ prolapse is lacking.
III. Dong Quai:
Dong quai, also known as female ginseng, is an herb traditionally used in Chinese medicine for various women’s health issues. It is thought to have toning and strengthening properties that may benefit the pelvic floor. However, further research is needed to determine its effectiveness specifically for pelvic organ prolapse.
It is important to exercise caution when using herbal remedies and consult with a healthcare professional before incorporating them into your treatment plan. Herbal remedies can interact with medications and may not be suitable for everyone, particularly those with underlying health conditions.
D. Acupuncture and Physical Therapy:
Alternative therapies such as acupuncture and physical therapy may complement conventional treatments for pelvic organ prolapse. Acupuncture involves the insertion of fine needles into specific points of the body to promote healing and balance. It may help manage pain associated with prolapse and improve overall well-being. Physical therapy techniques, such as myofascial release and trigger point therapy, can also be beneficial in addressing pelvic floor muscle dysfunction and reducing symptoms.
These natural solutions can provide additional support and help improve symptoms for individuals with pelvic organ prolapse. However, it is important to remember that natural remedies should not replace or delay seeking professional medical advice. Consulting with a healthcare professional experienced in pelvic floor disorders will ensure a comprehensive and individualized approach to managing pelvic organ prolapse.
Combining Conventional and Natural Approaches
For individuals with pelvic organ prolapse, combining conventional medical treatments with natural approaches can often yield the best outcomes. Integrating these different approaches allows for a comprehensive and personalized treatment plan tailored to specific symptoms and needs. Collaboration with healthcare professionals is essential to ensure safe and effective management.
Here’s a further explanation of combining conventional and natural approaches:
By combining conventional and natural approaches, individuals with pelvic organ prolapse can benefit from a holistic treatment plan that addresses both the physical and lifestyle aspects of their condition. Here are some key considerations:
I. Collaboration with healthcare professionals:
It is crucial to work closely with healthcare professionals who specialize in pelvic floor disorders. They can assess the severity of the prolapse, guide the use of conventional treatments, and provide expert advice on incorporating natural approaches. These professionals can monitor progress, make adjustments to the treatment plan as needed, and ensure that the chosen natural remedies do not interfere with any medications or other treatments.
II. Personalized treatment plans:
Each person’s experience with pelvic organ prolapse is unique, and treatment plans should be tailored to individual symptoms and needs. The combination of conventional and natural approaches can be customized to address specific concerns, such as pelvic floor muscle weakness, lifestyle modifications, or herbal remedies. Healthcare professionals can guide you in selecting appropriate exercises, recommending specific dietary modifications, or suggesting herbal remedies with potential benefits.
III. Safety and efficacy:
While natural approaches can provide additional support, it is important to prioritize safety and ensure their efficacy. Natural remedies should be thoroughly researched and discussed with healthcare professionals before incorporating them into the treatment plan. This helps ensure that the chosen remedies are safe, suitable for the individual’s specific condition, and do not interfere with any medications or conventional treatments.
IV. Monitoring and adjusting the treatment plan:
Regular follow-up appointments with healthcare professionals are essential to monitor progress and make any necessary adjustments to the treatment plan. This ongoing collaboration allows for the evaluation of symptom improvement, reassessment of prolapse severity, and modification of exercises, lifestyle modifications, or natural remedies as needed.
Combining conventional and natural approaches for pelvic organ prolapse offers a comprehensive approach that considers both medical interventions and lifestyle modifications. By integrating the strengths of each approach, individuals can benefit from improved symptom management, enhanced quality of life, and better overall pelvic floor health.
It is important to note that the effectiveness of natural remedies may vary from person to person, and they may not be suitable or effective for everyone. Healthcare professionals can provide individualized guidance and ensure that the chosen combination of treatments aligns with the specific needs and preferences of each individual.
Remember, an informed and collaborative approach with healthcare professionals is key to developing a personalized treatment plan that combines conventional and natural approaches for optimal outcomes in managing pelvic organ prolapse.
Herbs for Health: Harnessing Nature’s Powerful Healing Power In 2023
Pelvic Organ Prolapse Treatments in Ayurveda
Pelvic organ prolapse is a condition that affects the pelvic floor muscles and supporting structures. Ayurveda, a traditional system of medicine originating from India, offers holistic approaches to managing various health conditions, including pelvic organ prolapse.
While it is important to consult with a qualified Ayurvedic practitioner for personalized advice, here are some general treatments that may be recommended in Ayurveda:
I. Panchakarma:
Panchakarma is a detoxification and rejuvenation therapy in Ayurveda. It involves a series of cleansing procedures to eliminate toxins and restore balance in the body. Panchakarma treatments may include specific therapies such as Basti (enema therapy) and Virechana (purgation therapy) to address imbalances in the pelvic area and improve overall pelvic floor health.
II. Herbal remedies:
Ayurveda utilizes a wide range of herbal remedies to support the body’s natural healing processes. Herbal formulations may be prescribed to strengthen the pelvic floor muscles, promote tissue health, and provide support to the organs. Examples of herbs commonly used in Ayurveda for pelvic organ prolapse include Ashoka, Lodhra, Shatavari, and Guggulu. These herbs are believed to have toning, strengthening, and rejuvenating properties that may help alleviate symptoms and support pelvic floor health.
III. Dietary modifications:
Ayurveda emphasizes the importance of a balanced diet in promoting overall health and well-being. Specific dietary recommendations may be provided to support pelvic floor health and prevent aggravation of symptoms. These recommendations may include incorporating foods that are nourishing, easy to digest, and supportive of the pelvic area. Ayurvedic practitioners may also suggest avoiding foods that are heavy, greasy, or difficult to digest, as they can contribute to imbalances in the body.
IV. Yoga and Pranayama:
Ayurveda often integrates yoga and pranayama (breathing exercises) as part of a holistic approach to wellness. Certain yoga asanas (postures) and pranayama techniques may be recommended to strengthen the pelvic floor muscles, improve circulation in the pelvic area, and enhance overall body-mind balance. Practices like Mula Bandha (root lock) and Ashwini Mudra (horse gesture) may be particularly beneficial for pelvic floor health.
V. Lifestyle modifications:
Ayurveda emphasizes the importance of lifestyle modifications in managing health conditions. Ayurvedic practitioners may guide in adopting a healthy daily routine, managing stress levels, and incorporating relaxation techniques. Stress reduction techniques such as meditation, deep breathing exercises, and adequate rest can support the body’s healing process and promote overall well-being.
It is important to note that Ayurvedic treatments for pelvic organ prolapse should be individualized based on an assessment of the person’s unique constitution (dosha), overall health, and specific symptoms. It is advisable to consult with a qualified Ayurvedic practitioner who can provide personalized recommendations and oversee the treatment process.
Furthermore, it is important to integrate Ayurvedic treatments under the guidance of a healthcare professional and in conjunction with conventional medical care. This allows for a comprehensive approach to managing pelvic organ prolapse and ensures that all aspects of your health are considered.
Pelvic Organ Prolapse Treatment With Kegels
Kegel exercises are commonly recommended as a non-surgical treatment option for pelvic organ prolapse. These exercises target the pelvic floor muscles, which play a crucial role in supporting the pelvic organs. Performing Kegel exercises correctly and regularly can help strengthen these muscles, improve their tone, and potentially alleviate symptoms associated with pelvic organ prolapse.
Here’s a detailed explanation of how Kegels can be used in the treatment of pelvic organ prolapse:
I. Locating the pelvic floor muscles:
The first step in performing Kegel exercises is to locate the pelvic floor muscles. To do this, imagine trying to stop the flow of urine midstream. The muscles you engage to achieve this sensation are the pelvic floor muscles. It’s important to note that once you’ve identified the muscles, you should not regularly interrupt the flow of urine during urination, as it can disrupt normal bladder function.
II. Proper technique:
To perform Kegel exercises, follow these steps:
- Sit, lie down, or stand in a comfortable position.
- Contract your pelvic floor muscles by squeezing or lifting them inward and upward.
- Hold the contraction for a few seconds, typically around 3 to 5 seconds, without holding your breath or tensing other muscles.
- Release the muscles and rest for a similar duration.
- Repeat the exercise, gradually increasing the duration of the contraction and relaxation as you become more comfortable.
III. Setting a routine:
Consistency is key when it comes to Kegel exercises. Aim to perform them at least three times a day, gradually increasing the number of repetitions and duration of each contraction over time. Start with a lower number of repetitions, such as 10, and gradually work your way up to 20 or more repetitions per session.
IV. Progression and maintenance:
As your pelvic floor muscles strengthen, you can progress to more advanced variations of Kegel exercises. This may include holding contractions for longer durations or performing quick, rapid contractions followed by longer holds. It is important to maintain a regular exercise routine to sustain the strength and tone of the pelvic floor muscles.
V. Supervision and guidance:
While Kegel exercises can be performed independently, it is advisable to seek guidance from a healthcare professional, such as a physical therapist specializing in pelvic floor rehabilitation. They can provide specific instructions, assess your technique, and offer personalized advice on incorporating Kegels into your overall treatment plan.
It’s important to note that Kegel exercises may not be suitable for everyone or may not be the sole treatment option for more severe cases of pelvic organ prolapse. Individualized guidance from a healthcare professional is crucial to ensure the exercises are appropriate for your condition and are performed correctly. In some cases, additional treatments, such as pessaries or surgery, may be necessary to manage pelvic organ prolapse effectively.
Remember to consult with a healthcare professional, preferably one specializing in pelvic floor disorders, to receive a comprehensive evaluation and personalized recommendations based on your specific needs. They can guide you on incorporating Kegel exercises into your treatment plan and suggest other suitable interventions if needed.
Prevention Tips
While pelvic organ prolapse cannot always be completely prevented, adopting certain measures can help reduce the risk or delay its onset. By incorporating the following prevention tips into your lifestyle, you can promote pelvic floor health and potentially minimize the chances of developing pelvic organ prolapse.
Here are some detailed explanations and examples:
I. Maintaining a healthy weight:
Maintaining a healthy weight is important for overall health and can positively impact pelvic floor health. Excess weight can place additional strain on the pelvic floor muscles and weaken the supportive structures, increasing the risk of prolapse. By maintaining a healthy weight through a balanced diet and regular exercise, you can reduce the burden on the pelvic floor and minimize the risk of developing or worsening pelvic organ prolapse.
II. Practicing good posture and body mechanics:
Poor posture and improper body mechanics can contribute to increased pressure on the pelvic floor and potentially worsen pelvic organ prolapse. Maintaining good posture, both while sitting and standing, helps distribute the weight evenly and reduces strain on the pelvic floor. It is important to be mindful of your body alignment and engage in activities that promote good posture to minimize the risk of pelvic organ prolapse.
III. Avoiding heavy lifting or using proper lifting techniques:
Heavy lifting can strain the pelvic floor muscles and weaken the supportive structures, increasing the risk of prolapse. Avoiding or minimizing heavy lifting can help prevent excessive pressure on the pelvic floor. If lifting heavy objects is necessary, using proper lifting techniques, such as bending the knees, lifting with the legs, and avoiding straining the pelvic floor, can help minimize the risk of injury and reduce the strain on the pelvic floor.
IV. Quitting smoking:
Smoking has been associated with a higher risk of pelvic organ prolapse. Chronic coughing caused by smoking can weaken the pelvic floor muscles and increase intra-abdominal pressure, contributing to the development or worsening of prolapse. Quitting smoking can not only benefit overall health but also reduce the strain on the pelvic floor and potentially lower the risk of pelvic organ prolapse.
V. Managing chronic coughing or constipation promptly:
Chronic coughing and constipation can strain the pelvic floor and potentially lead to or exacerbate pelvic organ prolapse. Managing these conditions promptly and effectively, such as through medical treatment or lifestyle modifications, can help prevent prolonged periods of strain on the pelvic floor muscles and reduce the risk of prolapse. Seeking medical attention and adopting appropriate strategies to manage chronic coughing or constipation are crucial preventive measures.
While these prevention tips can help reduce the risk or delay the onset of pelvic organ prolapse, it is important to remember that they may not guarantee complete prevention. Some factors contributing to pelvic organ prolapse, such as genetics and hormonal changes, may be beyond our control. However, adopting these preventive measures can promote overall pelvic floor health and minimize the risk factors associated with pelvic organ prolapse.
If you have concerns about pelvic organ prolapse or want to learn more about preventive strategies, it is advisable to consult with a healthcare professional who specializes in pelvic floor disorders. They can provide personalized guidance and recommendations based on your individual needs and circumstances.
The V-Core Lift Essential Program (TM)
Pelvic and Bladder Healing
1. Empowerment Strategies for Pelvic Vitality & Power
Gain control over your pelvic health and bid farewell to issues like pee leaks, pressure, and numbness. In Module 1, we provide you with the necessary tools to transform your everyday behaviors and achieve long-lasting healing. Let’s explore the fundamental aspects of this module:
I. Overcoming Pelvic Imbalance and Suffering
- Uncover the roots of your bladder and pelvic symptoms, allowing you to make the essential lifestyle changes that promote healing and restore balance.
II. Connecting with Your Body’s Messages
- Develop a deeper understanding of your body’s signals and symptoms, empowering you to implement changes that target the root causes of your pelvic issues.
III. Exploring Breath Work and Guided Meditation
- Tap into the power of breathwork and guided meditation to connect with your inner wisdom and embrace your feminine essence.
IV. Enhancing Posture and Movement Patterns
- Discover the significance of proper posture and movement in restoring the strength of your pelvis and achieving bladder control.
V. Unleashing the Untapped Power of the Female Body
- Unlock the potential of your body to experience more joy, conquer fear, and foster a sense of freedom and empowerment in all aspects of your life.
2. Discovering the Strength of Your Pelvic Floor
Module 2 offers an in-depth exploration of your pelvic floor, providing you with a comprehensive understanding of its functionality and strength. As you delve into this module, you will gain the knowledge necessary to take charge of your physical well-being. Let’s delve into the key highlights:
I. Understanding the Anatomy of the Pelvic Floor
- Familiarize yourself with the different levels and anatomy of the pelvic floor, enabling you to develop pelvic power, bladder control, and awareness.
II. Shifting Your Knowledge for Personal Empowerment
- Empower yourself by acquiring the knowledge required to manage your physical well-being, eliminating the need to rely on external sources for your care.
III. Assessing the Strength of Your Pelvic Floor
- Discover methods to assess the strength of your pelvic floor and learn strategies to enhance comfort, confidence, and stability in your pelvis and life.
IV. Unraveling the Secrets of Your Pelvic Region
- Gain insights into the true nature of your pelvic region and learn how to harness its power to elevate your life force, happiness, and overall well-being.
3. Rejuvenating Your Pelvic Floor & Bladder: The Kegel Series
Unlock the full potential of your pelvic floor and bladder to restore pelvic health naturally. Module 3 introduces you to various types of Kegels and the transformative Un-Kegel technique. Here’s what you can expect from this module:
I. Healing Leaking, Prolapse, and Diminished Sensation
- Explore the effectiveness of different Kegels and Un-Kegels in addressing common issues like urinary leakage, prolapse, and reduced sensation. Regain control over your pelvic health, well-being, and joy.
II. Empowering Yourself with Correct Kegel Techniques
- Learn simple yet powerful ways to perform Kegels correctly, enabling you to alleviate the symptoms that disrupt your life.
III. Unlocking Vaginal Tensions and Traumas
- Activate your capacity to identify and release long-held vaginal tensions and traumas stored in your pelvis, fostering a healthier and more harmonious relationship with your body.
IV. Breaking Free from Unhealthy Habits
- Break free from recurring Kegel habits that hinder your health and prevent you from embracing a vibrant and fulfilling life.
V. Cultivating a Deep Understanding of Your Body
- Develop a profound connection with your body, creating harmony within yourself and fostering balanced and healthy relationships with others.
4. Repairing and Strengthening Your Core: Crunchless Core
Leave behind ineffective exercise routines and embark on a journey to enhance your abdominal strength while prioritizing pelvic floor safety. In Module 4, you will learn proven abdominal exercises that flatten your tummy and amplify the power of your pelvic floor. Additionally, we’ll address the issue of Diastasis Recti Separation, also known as the “Mummy Tummy.” Let’s explore the module’s highlights:
I. A Core Exercise Routine for a Confident You
- Discover a core exercise routine that can be conveniently performed at home, enabling you to improve your posture, appearance, and overall confidence.
II. Strengthening Your Abdominal Muscles
- Learn how to strengthen your abdominal muscles to provide essential support to your pelvic floor and organs while healing diastasis recti.
III. Body Positivity and Unconditional Self-Love
- Discover specific abdominal exercises that promote body positivity and foster an unwavering relationship with yourself, allowing you to embrace self-love unconditionally.
IV. Achieving the Desired Midsection and Flat Tummy
- Unleash a set of proven exercises that target your midsection, granting you the toned and flat tummy you’ve always desired.
5. Prevention: Healing Pelvic Organ Prolapse & Pressure
Step away from relying solely on medical professionals and embark on a journey of self-healing and empowerment. In Module 5, we explore the power of lifestyle changes and exercises in preventing and addressing issues like pelvic organ prolapse, pressure, and discomfort. Let’s dive into the key aspects of this module:
I. Embracing Symptoms as Opportunities for Healing
- Shift your perspective on symptoms and embrace them as opportunities for growth and self-healing.
II. Harnessing Feminine Intuition for Healing
- Tap into your innate feminine intuition to create lifestyle changes that support the healing and optimal positioning of your pelvic floor and organs.
III. Listening to Your Body’s Messages
- Develop the ability to interpret the messages your body sends, enabling you to make immediate changes that foster long-term healing.
IV. Tools for Personal Sovereignty and Healing
- Equip yourself with the necessary tools to reclaim your sovereignty, unlock your true essence, and experience profound healing results.
V. Trusting Yourself on the Path to Complete Healing
- Learn to address your symptoms with confidence, trusting that you now possess the knowledge and understanding needed to heal fully and live a life free from fear or inhibitions.
6. Reconnecting with Your Body: Body Work & Scar Healing Techniques
Discover the missing piece of the pelvic floor-bladder puzzle and embark on a journey to care for your body holistically. In Module 6, you will uncover the secrets of bodywork, fascia, and scar healing techniques, allowing you to create a pain-free body that works in harmony with your goals. Here’s what awaits you in this module:
I. Self-Massage for Pain Relief and Healing
- Master the art of a simple self-massage that alleviates scar pain, body pain, and excessive urination, granting you a newfound sense of freedom.
II. Purposeful Touch for Self-Liberation
- Learn how to touch your body intentionally, fostering a deep connection and setting yourself free from limitations.
III. Embracing Your Unique Body
- Release the need for comparison and embrace the uniqueness of your body, appreciating its beauty and strength.
IV. Integrating Previous Modules into Your Journey
- Integrate the knowledge and insights gained from previous modules into your journey, creating a holistic approach to pelvic health and well-being.
V. The Power of Bodywork and Self-Empowerment
- Recognize the significance of bodywork as a gateway to self-empowerment, embracing your unbreakable female body and pelvic floor.
Embrace Pelvic and Bladder Healing
The path to pelvic and bladder healing is within reach, and with our comprehensive modules, you can embark on a transformative journey toward complete recovery. From understanding the underlying causes of pelvic issues to reclaiming your body’s power, each module equips you with the knowledge and tools needed to restore balance and vitality. Through empowering strategies, exercises, and self-care techniques, you can overcome leaking, discomfort, and other symptoms that have hindered your quality of life.
Remember, you are not alone in this journey. Our program offers a supportive community where you can connect with others who are also on the path to healing. Together, you can share experiences, and insights, and celebrate victories, fostering a sense of empowerment and sisterhood.
Don’t wait any longer to take control of your pelvic and bladder health. Log into your account, access the modules, and unlock the potential for a life free from limitations. The power to heal is within you, and our program is here to guide you every step of the way.
Embark on this empowering journey today and discover the true strength and resilience of your pelvic floor.

Above program is written and being operated by Mrs. Isa Herrera, MSPT, CSCS, a licensed, pelvic physical therapist. For the last 15 years, who have personally helped over 15,100 women resolve their symptoms naturally in my NYC Madison Ave clinic.
Conclusion
Pelvic organ prolapse is a common condition that affects many women, causing discomfort and impacting their quality of life. Understanding the causes, symptoms, and treatment options is crucial in managing this condition effectively.
While conventional treatments such as lifestyle modifications, pelvic floor exercises, pessaries, and surgery are available, natural solutions like pelvic floor muscle training, healthy lifestyle practices, herbal remedies, acupuncture, and physical therapy can also provide additional support.
It is important to consult with healthcare professionals to determine the most suitable treatment plan based on individual needs and preferences.
FAQs
Q. Can pelvic organ prolapse resolve on its own without treatment?
A. While some cases of mild prolapse may improve on their own, most cases require treatment to manage symptoms and prevent further complications.
Q. Can exercises worsen pelvic organ prolapse?
A. When performed correctly, pelvic floor exercises can help strengthen the muscles and improve prolapse symptoms. It is essential to learn the proper technique from a qualified healthcare professional.
Q. Are there any non-surgical alternatives to treat pelvic organ prolapse?
A. Yes, non-surgical options like lifestyle modifications, pelvic floor exercises, and pessaries can provide relief and improve the quality of life for individuals with pelvic organ prolapse.
Q. Are there any long-term consequences of untreated pelvic organ prolapse?
A. Untreated pelvic organ prolapse can lead to worsening symptoms, decreased quality of life, and potential complications such as urinary or bowel dysfunction.
Q. Can men develop pelvic organ prolapse?
A. Although rare, men can also develop pelvic organ prolapse, especially if they have undergone prostate surgery or have conditions that weaken the pelvic floor muscles.

daxktilogibigibi.NttCkUYCFVrv